Dr. Bradley received her doctorate from the University of California Berkeley, in 1981 in studies of CD4 T cell subsets that regulate humoral immune responses. Her work on the regulation of CD4 T cells continued during her postdoctoral training at The Oregon Primate Research Center and at the University of California, San Diego where she was appointed Assistant Research Professor in 1991. It was at this time she developed NIH sponsored her research program on CD4 T cells and discovered the key associations between migration and function. She joined The Scripps Research institute as an Assistant Professor in 1996 where she expanded her work on CD4 T cells into the arena of autoimmunity and discovered the essential role of the cytokine, interleukin-7, in the regulation of CD4 cell homeostasis.
She joined the Sidney Kimmel Cancer Center in 2001 as an Associate Professor, and was promoted to Professor in 2005. She joined Sanford Burnham Prebys as a Professor in the Infectious and Inflammatory Diseases Center in 2009. Dr. Bradley is recognized as a key contributor in the field of CD4 T cell biology, is an invited speaker at many national and international meetings, and serves on several study sections for the NIH as well as the Welcome Trust, Medical Research Council, and the JDRF.
Related Disease
Cancer, Infectious Diseases, Skin Cancer and Melanoma
Phenomena or Processes
Adaptive Immunity, Cell Signaling, Infectious Disease Processes, Inflammation
Anatomical Systems and Sites
Immune System and Inflammation
The research program in the Bradley lab is focused on understanding the regulation of T lymphocytes in virus infections where the immune response results in viral clearance and the development of immunologic memory, and in chronic virus infections where the ongoing immune response leads to viral persistence and immune dysregulation. They are guided by these studies to interrogate cellular mechanisms that can be modulated to promote better responses not only to virus infections, but also to relieve immune inhibition in the setting of cancer where T cells progressively lose function. Understanding adhesion mechanisms underlie the ability of T cells to become localized in tissues to eradicate infections and tumors is a key underpinning of their work.
The Bradley lab’s current focus is on two molecules that can function on T cells to initiate the processes that lead to their migration from the blood into tissue, CD44 and PSGL-1 (P-selectin glycoprotein-1). They have found that both of these receptors have key regulatory functions that are independent of their roles in migration. These proteins regulate the magnitude of T cell responses, as well as the survival and memory formation by T cells by different mechanisms, affecting processes in the T cell and stromal cell compartments.
Their ongoing studies of these immune checkpoint regulators using in vivo models indicate that they are promising therapeutic targets to enhance T cell responses to infections and cancer as well as to inhibit T cell responses in autoimmunity. They are therefore pursuing translational studies with the UCSD Moores Cancer center to analyze their regulation in human T cells in an effort to enhance patient responses to their tumors using in vivo modeling. In addition working to develop biologics for treatment of patients with autoimmunity and cancer.
 Aug 19, 2024
Aug 19, 2024Women in Science event at Sanford Burnham Prebys examines how female faculty members navigate research careers
Aug 19, 2024Topics at the event included work/life balance, caregiving and family obligations, and gender disparities in academic rank at research and…
 Mar 26, 2024
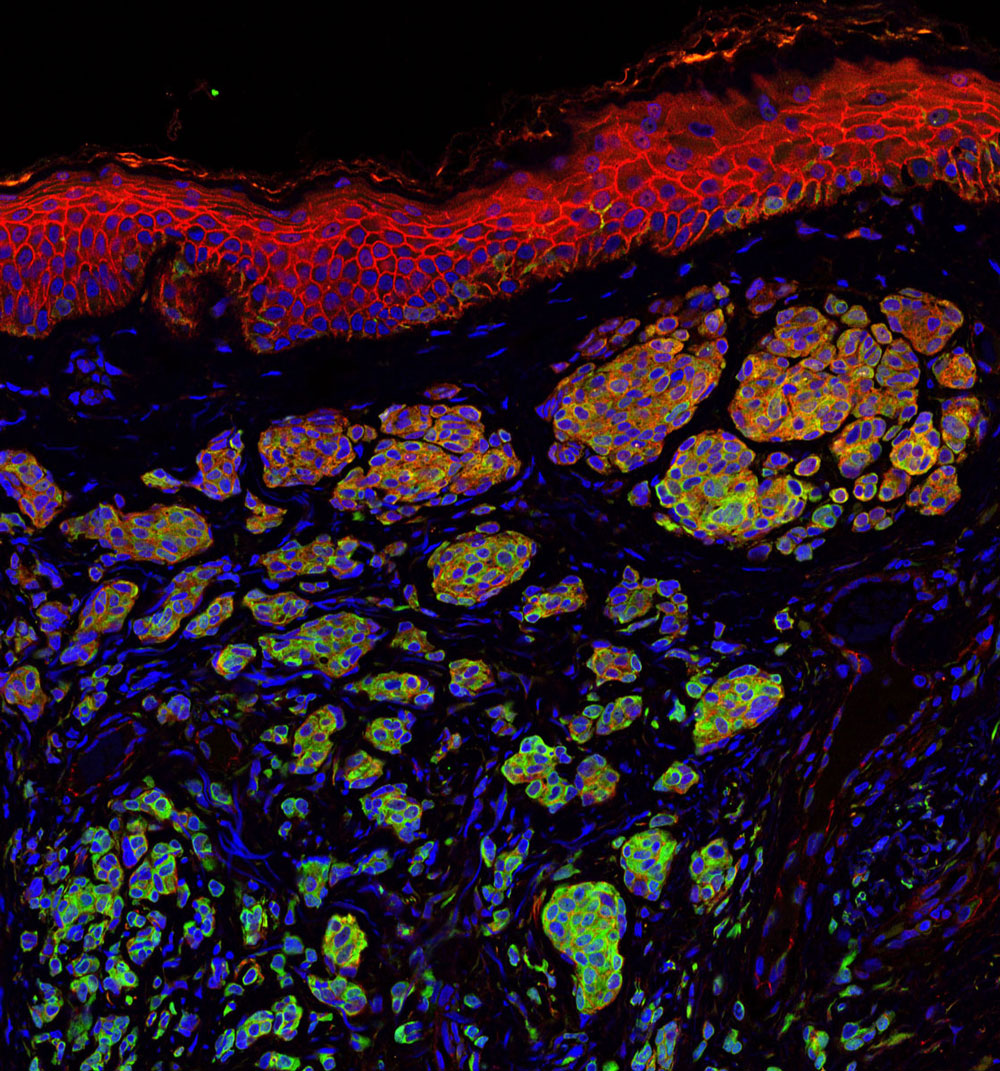
Mar 26, 2024Melanoma’s mysteries revealed at Sanford Burnham Prebys
Mar 26, 2024Cancer Center open house welcomes San Diego community to learn the latest about melanoma research.
 May 3, 2023
May 3, 2023Reviving exhausted T cells to tackle immunotherapy-resistant cancers
May 3, 2023A new approach to immunotherapy could help overcome treatment resistance in cancer. When the cells of our immune system are…
 Mar 20, 2023
Mar 20, 2023Sanford Burnham Prebys researchers awarded Curebound grants
Mar 20, 2023Each year, Sanford Burnham Prebys joins Padres Pedal the Cause, an annual fundraising event that raises money for Curebound which…
- Mar 19, 2018
Cancer immunology symposium highlights hot area in cancer research
Mar 19, 2018The Cancer Immunology and Tumor Microenvironment Symposium held at Sanford Burnham Prebys Medical Discovery Institute (SPB) on March 8, 2018…
 May 16, 2017
May 16, 2017What SBP Scientists are Researching to Battle Skin Cancer
May 16, 2017Skin cancer is one of the most common of all cancers, and melanoma accounts for about 1 percent of skin…